Author: Liliana Sánchez Rocha
Read time: 5 minutes
Mycobacterium tuberculosis, the driving force behind Tuberculosis has been lurking around on earth for the past 3 million years, evolving and developing sinister mechanisms to outsmart any attack. Its mission? SURVIVE, no matter the cost of human lives. In just the last two centuries 1 billion souls have been slowly consumed by this merciless creature, which is more than all pandemics combined! There was hope when its identity was exposed in 1882, bringing plenty of opportunities to counterattack and protect humanity. Although it has been kept at bay in many countries, TB continues to claim lives worldwide. In 2022, it killed 1.3 million people! Not impressed? imagine 12 fully loaded jumbo jets crashing every single day! But now, the world faces another challenge in the fight against this ancient serial killer. The misuse of antibiotics is giving rise to new super potent generations of this bacteria with higher infection power and even worse; resistance to the few drugs available to destroy it. Are we facing a potentially indestructible enemy?

What is tuberculosis and why do you get it?
Let’s start from the beginning, tuberculosis (TB) is a serious infectious disease caused by the bacteria Mycobacterium tuberculosis (M. tuberculosis). This sneaky creature mainly affects the lungs, although it can also move to other organs such as your kidneys, spine, or brain. But how can you get tuberculosis? People having an active infection (when the bacteria is busy multiplying), can expel M. tuberculosis in tiny particles of liquid (droplets) during a sneeze or while coughing. As if the droplets were private jets, they propel this mycobacterium to an unsuspecting victim, who breads in the droplets and gives M. tuberculosis free entrance to begin its conquest.
The silent invasion of M. tuberculosis
Once in the respiratory system, the bacteria find their way into the smallest corners of the lungs (alveoli), but M. tuberculosis is not here to escape or hide. No! It’s here to carry out its master plan of deception and manipulation. When the presence of this intruder is sensed by the vigilant macrophages (giant immune cells), without hesitation these immune cells mold their body to tightly surround the uninvited guests. In an unfriendly hug, the little M. tuberculosis are aggressively squeezed into the insides of the big body of the macrophage. Once in the macrophage’s gut, any other intruder is fused to a cellular compartment… imagine it as a bubble, where chemicals mix to create an acidic cocktail that leaves nothing but “ashes”. However, M. tuberculosis is just not ANY intruder, there is a reason it has been around for thousands of years! It “knows” the trick, and it’s up for the fight!
While the clueless macrophage continues its patrol, M. tuberculosis uses its MacGyver-like tricks to avoid the fatal fusion with the “acidic party bubble” and silently breaks free inside the macrophage’s gut. This fascinating escape allows M. tuberculosis to go under the radar and provides it with ample resources and time to replicate. It is not until the macrophage has been consumed from inside that it ends up exploding! splashing guts, DNA, bacteria, and debris in the alveoli. The immune alarms go off and many more macrophages come to the “crime scene”, but this, just as before is just part of the plan, because those macrophages will be parasitized and devoured alive.
As more macrophages explode, damaging elements (intended to kill invaders) are released, harming the lungs. This chaos calls in specialized immune cells (lymphocytes) to contain the attack. As if it were a tactic of war, the lymphocytes warriors, and other immune cells form a thick and tight line of defense around the damaged area, ready to die before letting the mycobacteria escape. This combat zone made out of M. tuberculosis, monocyte´s corpses, and decaying matter surrounded by this barely “living wall” is known as granuloma. If your immune system is healthy, you might win this war, or your body might believe so, because then M. tuberculosis will resort to “play dead” and patiently await until the army weakens. Although it is confined in the granuloma, it is also protected and can survive for decades! This is known as a “latent infection”. It has been estimated that almost a quarter of the planet might carry this sneaky creature in the “silent mode”, 1 in 4 people! Could you be… THE ONE? If so, remain vigilant to any severe disease, like HIV, or any situation that weakens your immune defenses, because then you are up for some serious granuloma explosion! Where all the putrefied cheese-like content will promote destruction in your lungs (seriously, it looks like cheese!). As more M. tuberculosis escape, some will be propelled to the outside world to infect other people, and some mycobacteria might travel through your body to colonize other organs, slowly making a fondue out of your body, the favorite snack of Mr. Black!
Tuberculosis symptoms
Have you lost a lot of weight, feel weak, sweat at night, have fever, chest pain, prolonged coughs, or even cough up blood? Beware! You could be in danger! However, keep in mind that symptoms can vary greatly and will depend on the organ that is under attack.
Tuberculosis test
There are many tests that can reveal if you have been in contact with M. tuberculosis, for instance, the tuberculosis skin test (Mantoux) or the blood test (IGRA). You could also get a chest X-ray to discover if there are any granulomas in your lungs. In case any of these tests is positive you must be immediately treated, even if you don’t have symptoms yet (latent infection).
The dark side of the resistance
As M. tuberculosis can be shielded within the granulomas, treatments do not easily trespass this barrier, which requires a strong, savage, and permanent ambush. That is why TB treatments might take 4, 6, or even 9 months! depending on the patient. Unfortunately, there are just four types of drugs able to unarm TB, and due to antibiotic misuse, and other complex factors, a fierce multi-drug-resistant M. tuberculosis is arising. Is everything lost? Researchers are working hard to develop medicines and make treatments shorter, but meanwhile, we all can contribute to this battle by remaining vigilant of our own health, do not misusing antibiotics, following the expert’s advice, do not sneezing on people’s faces! And share this fascinating story, because now you know the enemy and have uncovered its deceiving disguise!
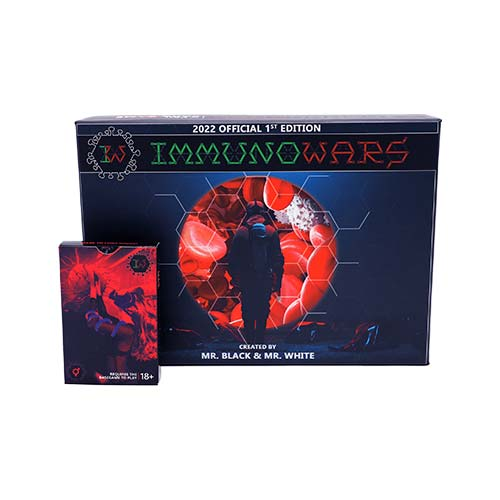
Gameplay Guide: Attack with Tuberculosis in ImmunoWars

When playing in the ImmunoWars field, you can choose two different tactics while using the tuberculosis card. For 3 ATP you will cause granulomas in your opponent’s lungs, costing them 1 health point (HP)/turn for 3 rounds. However, if your opponent is building a strong immune strategy (with monocytes, B-cells, Dendritic cells, T cells…) then this is your opportunity to take them down! For 5 ATP you could dismantle their immune system by giving them an extrapulmonary disease and thus making them lose one of their immune soldiers each round. During 3 agonizing turns, you will enjoy their painful loss. No immune defense yet? no problem, they’ll lose instead 2HP per turn, making their downfall even quicker. Watch out! this card has 3 contagiousness, marked by biohazard circles in the bottom left corner of the card. If you want to attack the same player with another disease then you run the risk to co-infect yourself! Is it worth the risk?
How to counterattack? Tuberculosis has a severity of 2, as indicated by the 2 stars in the bottom right corner. Therefore, you'll need a Consumable or Immunocard that can treat Bacteria of at least 2 stars. If you are already in intensive care due to multiple infections, then you can always resource to drink some bleach, you will wipe out all diseases, BUT WAIT! it will come at a high cost! The choice is yours, just remember that no one is safe in this game! Get ImmunoWars here.
References
Barberis I, Bragazzi NL, Galluzzo L, Martini M. The history of tuberculosis: from the first historical records to the isolation of Koch's bacillus. J Prev Med Hyg. 2017 Mar;58(1):E9-E12. PMID: 28515626; PMCID: PMC5432783.
World Health Organization: WHO. Tuberculosis [Internet]. 2019. Available from: https://www.who.int/health-topics/tuberculosis#tab=tab_1
Dheda, K., Mirzayev, F., Cirillo, D.M. et al. Multidrug-resistant tuberculosis. Nat Rev Dis Primers 10, 22 (2024). https://doi.org/10.1038/s41572-024-00504-2
Zhai W, Wu F, Zhang Y, Fu Y, Liu Z. The Immune Escape Mechanisms of Mycobacterium Tuberculosis. Int J Mol Sci. 2019 Jan 15;20(2):340. doi: 10.3390/ijms20020340. PMID: 30650615; PMCID: PMC6359177.
Singh V. Tuberculosis treatment-shortening. Drug Discov Today. 2024 May;29(5):103955. doi: 10.1016/j.drudis.2024.103955. Epub 2024 Mar 26. PMID: 38548262.
Houben RMGJ, Dodd PJ. The Global Burden of Latent Tuberculosis Infection: A re-estimation using Mathematical modelling. PLoS Medicine [Internet]. 2016 Oct 25;13(10):e1002152.
World Health Organization: WHO, World Health Organization: WHO. Tuberculosis [Internet]. 2023. Available from: https://www.who.int/news-room/fact-sheets/detail/tuberculosis
Preventing tuberculosis [Internet]. Tuberculosis (TB). 2024. Available from: https://www.cdc.gov/tb/prevention/index.html