Author: Liliana Sánchez Rocha
Read time: 7 minutes
In our introductory article, we learned that Escherichia coli are normally the good guys; helpful, peaceful residents of your gut, aiding digestion like tiny food processors. But, as with any large family, not all members play nice. The E. coli clan, with its hundreds of relatives, also includes bad guys. Some have mastered devious tricks, transforming from friendly neighbors into vicious invaders. In the first chapter, we’ve taken you through the genetic secrets they use to turn to the pathogenic dark side. But we have yet to discover the implications of their change of heart. In this episode, we´ll explore E. coli's destructive nature; what diseases they cause, and most importantly, how to avoid becoming their next victim, or… can we really avoid it?

Can E. coli cause disease?
Yes! It is important to note that although most E. coli play by the rules and stay confined to your gut, they should not be underestimated. If these usually harmless bacteria wander off to places they don’t belong, like your urinary tract or bloodstream, they’ll grab the opportunity to disturb the peace and become tyrants. Your own E. coli can invade your body through, well... not-so-pleasant routes, like fecal contamination. Forgetting to wash your hands after a bathroom break? This mistake gives E. coli the perfect chance to jump ship from gut to mouth or urethra, causing you a very painful regret. Another not very common track of E. coli to escape the gut, is if your intestinal wall springs a leak. They’ll escape like bandits, causing septicemia and turning your body into a battleground, fortunately, this is not so common. Some other times, your microbiota may experience changes that result in a sudden E. coli uprising. If your immune system can’t contain this change in the forces; cramps, vomiting, and diarrhea can take over until the forces are restored.
Where do pathogenic E. coli come from?
Aside from the resident E. coli that occasionally bothers your body, a group of dangerous E. coli subtypes can cause very serious diseases. Mostly intestinal, but sometimes infections can disseminate to the kidneys and even to the brain, threatening the patient’s life. These pathogenic gangs can develop in the comfort of the bowel of a person or animals but also out in nature. One of the most problematic E. coli variants develops in healthy cattle. But how do these dangerously equipped forms find their way to their victims?
How is E. coli transmitted?
After being excreted into the environment, E. coli can not only survive but also grow for the first three days. Although its numbers eventually decline, it survives long enough to spread its mischief. That fecal matter can run off into water, contaminate vegetables, or worse; it finds its way into the meat we eat. This can happen due to bad hygienic practices. All it takes is one bite of undercooked beef, one glass of unpasteurized milk, or even some poorly washed veggies, and the bacteria are in, waiting to create chaos.
Which are the pathogenic forms of E. coli?
There are six well-known types of E. coli that specialize in causing diarrhea, each with its own set of sneaky tactics. At the end, we will focus on the enterohemorrhagic (EHEC) type, one of the most problematic and dangerous.
- EHEC/STEC: Enterohemorrhagic: Our main star, causing severe diarrhea, cramping, and sometimes kidney failure.
- ETEC: Enterotoxigenic: The sneaky traveler’s diarrhea culprit. It latches onto your gut, releasing toxins that make you wish you never left home.
- EPEC: Enteropathogenic: Lurks in babies, especially in developing countries, causing severe diarrhea.
- EIEC: Enteroinvasive: In a ninja-move quietly invades and destroys the cells that form your gut lining. It causes bloody diarrhea.
- EAEC: Enteroaggregative: E. coli gathers in groups and produces toxins, causing persistent diarrhea. Usually self-limiting in 3 to 4 days.
- DAEC: Diffusely adherent: The clingiest of them all. It sticks to your intestinal cells and causes prolonged diarrhea, especially in kids.
Enterohemorrhagic E. coli EHEC/ STEC
E. coli enterohemorrhagic, has been the star and main character of multiple outbreaks across the globe. The most representative individual of this group is known as O157:H7 (for its molecular characteristics). O157:H7 hit the headlines in 1982, thanks to an outbreak linked to undercooked hamburgers in the U.S. This type (strain) thrives in the intestines of cattle, goats, and sheep. It can survive temperatures between 7°C and 50°C (dying for sure at 70°C). It takes just 10 to 100 bacteria to trigger a full-on internal war! Compared to the million-plus required by the other strains, there is no wonder why this is the celebrity of the pathogenic E. coli!
Its weapon of choice is the Shiga toxin, which sabotages your gut cells by cutting off their energy supply, killing them in the process. But it doesn’t stop there. Once it enters the bloodstream, it targets red blood cells, platelets, and even kidneys, potentially causing hemolytic uremic syndrome (HUS), a condition that can lead to kidney failure and brain damage. And the cruelest twist? Antibiotics, usually our go-to defense, can backfire with O157. Instead of killing the bacteria, they can trigger it to release even more toxins, worsening the patient’s condition.
What are the E. coli infection symptoms?
Once this E. coli enters the body, it’s a waiting game. Symptoms like fever, diarrhea, vomiting, and fatigue show up between 3 to 8 days later. Sometimes, the war rages so hard that the patient can develop bloody diarrhea. While most people recover within 10 days, children and the elderly are at greater risk for severe outcomes, with a case-fatality rate between 3% and 5%.
What is the main treatment for E. coli?
When E. coli strikes, hydration is your first line of defense! In most cases, the infection will pass on its own within a few days. But if symptoms persist more than three days, it's time to call in the doctor! It’s crucial to investigate the type of E. coli that has invaded your body before choose a treatment. Treating the wrong type of E. coli with antibiotics could be like tossing gasoline on a fire. So, resist the urge to self-medicate! And let's not forget, some strains have already leveled up with antibiotic resistance. Yes! some of these bugs are armed and ready for a fight. But we’ll save that nightmare for another article!
How to prevent E. coli?
E. coli lives within us, and is part of our microbiota (positive microbes living in the gut), we can’t eliminate it and we don’t want to eliminate it. However, dodging E. coli infections is all about good hygiene practices. The basic point is to keep your environment clean, especially places where food is prepared. Separate raw and cooked foods, and cook thoroughly, 70°C is your safe zone! Don’t forget to wash your hands before eating, after bathroom breaks, and after petting animals, their poop can be loaded with pathogenic E. coli. Don’t forget to Protect your water sources from contamination.
What’s Next?
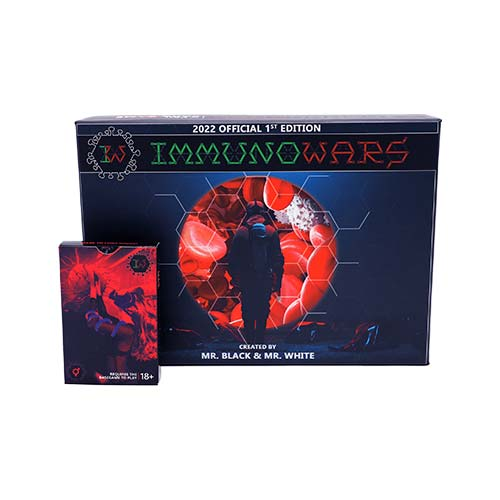
We’ve explored E. coli’s dark side, but this bacterium isn’t just a villain as we already know. Its rapid replication has made it a perfect model to study bacteria and discover life characteristics. This little hairy creature is behind the development of amazing technologies. Stay tuned for the next chapter to discover how E. coli has revolutionized science! Wait, If you want to know how to use the E. coli card as a weapon in immunoWars keep reading!
Gameplay Guide: Attack with E. coli in ImmunoWars
When you play this card, you’ve got two delightfully devious tactics to choose from.
- For just 3 ATP, your enemy will lose 2 health points (HP) in one round. In this hemorrhagic assault, no antibiotics can be used!
- For 5 ATP you can inflict a chronic anemia that lasts forever. Mwahaha! Your opponent will lose 2 ATP (energy) every single round.
This card has a contagiousness rating of 1, If you dare to attack the same player you might just co-infect yourself!
To fight off the first ability, you’ll need to make use of immunocards or action cards. For the second ability you can use medicine that tackles bacteria of at least 2 stars. Who’s ready to play? Get ImmunoWars here.
References:
- Rangel JM, Sparling PH, Crowe C, Griffin PM, Swerdlow DL. Epidemiology of Escherichia coli O157:H7 outbreaks, United States, 1982-2002. Emerg Infect Dis. 2005 Apr;11(4):603-9. doi: 10.3201/eid1104.040739. PMID: 15829201; PMCID: PMC3320345.
- Ameer MA, Wasey A, Salen P. Escherichia coli (e Coli 0157 H7) [Internet]. StatPearls - NCBI Bookshelf. 2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507845/
- Program HF. BAM Chapter 4A: Diarrheagenic Escherichia coli [Internet]. U.S. Food And Drug Administration. 2020. Available from: https://www.fda.gov/food/laboratory-methods-food/bam-chapter-4a-diarrheagenic-escherichia-coli
- World Health Organization: WHO. E. coli [Internet]. 2018. Available from: https://www.who.int/news-room/fact-sheets/detail/e-coli